Introduction
Childhood hypertension—once considered rare and almost exclusively an adult health issue—is now being recognized as a growing global public health concern. Recent research shows that high blood pressure in children and adolescents has nearly doubled in the past two decades, highlighting a trend that could have lifelong consequences if not addressed early and effectively.
What was once a health condition “too adult” for pediatric focus is now shifting into the spotlight of preventative medicine and child health advocacy. Indeed, a global review observed that rates of high blood pressure in children under age 19 increased from roughly 3% in 2000 to over 6% by 2020, representing tens of millions of affected young people worldwide.
1. Childhood Hypertension Is Increasing Worldwide

Over the past 20 years, the prevalence of hypertension among children and adolescents has nearly doubled globally. A large systematic review found that by 2020, about 6.2% of children under 19 qualified as having hypertension, up from around 3% in 2000.
Furthermore, nearly 8.2% of children are currently classified as having pre-hypertension, a condition in which blood pressure levels are elevated but have not yet reached the clinical threshold for hypertension. This intermediate stage is particularly concerning because it often progresses unnoticed without early screening or intervention. At the same time, prevalence estimates are known to vary across regions due to differences in diagnostic criteria, screening frequency, and blood pressure measurement techniques. Nevertheless, despite these methodological variations, research findings consistently point to a clear and sustained upward trend in elevated blood pressure among children worldwide.
Thus, what was once a minor pediatric health issue is now increasingly common, especially within populations exposed to certain lifestyle and environmental risk factors.
2. The Definition and Diagnosis Are Unique—and Often Misunderstood
Unlike adults, diagnosing hypertension in children is not based on a fixed number alone. Instead, hypertension is defined relative to percentile charts that account for age, sex, and height.
Key definitions used in the diagnosis of childhood hypertension are based on age-, sex-, and height-specific percentiles rather than fixed numerical thresholds. Elevated blood pressure, previously referred to as pre-hypertension, is defined as blood pressure readings at or above the 90th percentile but below the 95th percentile for a child’s age, sex, and height. Stage 1 hypertension is identified when readings fall at or above the 95th percentile up to less than the 95th percentile plus 12 mmHg, or, in some older adolescents, when measurements reach 130–139/80–89 mmHg. Stage 2 hypertension represents the most severe category and is diagnosed when blood pressure readings are at or above the 95th percentile plus 12 mmHg, or when values reach or exceed 140/90 mmHg in adolescents.
Moreover, at least three separate blood pressure measurements on different occasions are recommended to confirm a diagnosis, because blood pressure in children can vary more than in adults.
This complexity not only presents clinical challenges but also leads to underdiagnosis and misclassification, especially in settings where pediatric measurement protocols are not routinely followed. For example, a study in India found that single-visit measurements may dramatically overestimate hypertension prevalence, underscoring the need for multiple re-checks to ensure accuracy.
3. Lifestyle Factors Drive the Global Surge
While some cases arise from medically identifiable causes, such as heart, kidney, or endocrine disorders, the major drivers of rising childhood hypertension are modifiable lifestyle factors.
The main contributors include:
a. Obesity and Overweight
Children with obesity are significantly more likely to have elevated blood pressure. In some analyses, hypertensive rates reach nearly 20% among obese children, compared to just 3% among children of healthy weight.
b. Poor Diet
High salt intake, excessive consumption of processed foods, fast food diets, and sugary beverages collectively contribute to elevated blood pressure in children.
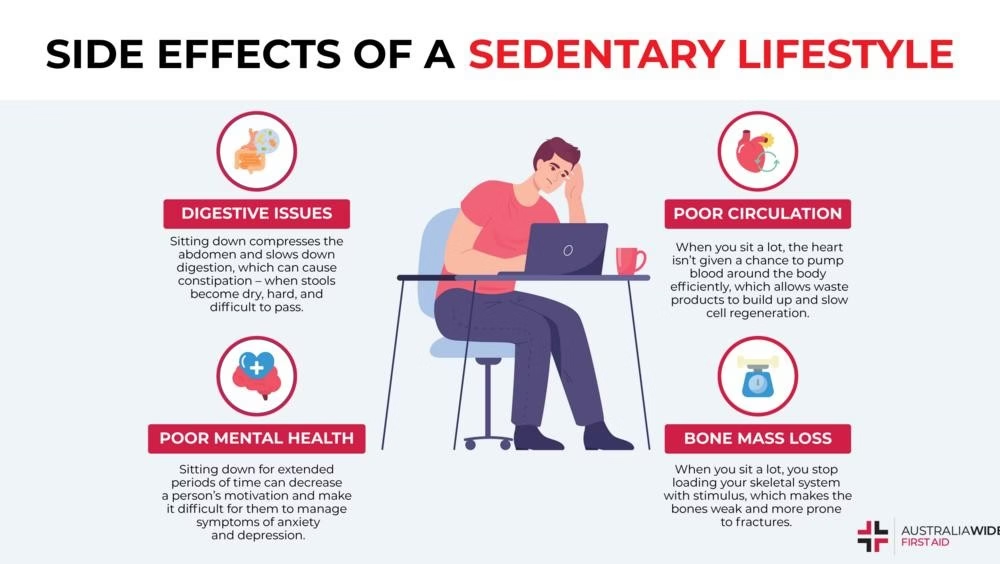
c. Sedentary Lifestyle
Reduced physical activity—often replaced by screen time—has been linked to both obesity and increased blood pressure readings in children.
d. Sleep Problems
Emerging research suggests that poor sleep quality and short duration may be associated with higher pediatric blood pressure outcomes.
Collectively, these lifestyle trends reflect broader societal shifts, including urbanization, changes in food systems, and digital engagement, which shape daily routines for children worldwide.
4. Long-Term Risks Are Significant but Largely Preventable

High blood pressure in childhood is not a “temporary childhood issue.” Rather, it sets the stage for adult health complications, if left unmanaged.
Link to Adult Disease
Children with elevated blood pressure are more likely to remain hypertensive into adulthood, increasing their risk for:
- Heart disease
- Stroke
- Kidney disease
- Early mortality
Additionally, evidence suggests that even moderately elevated childhood blood pressure can lead to subclinical cardiovascular changes, such as left ventricular hypertrophy, which are precursors to heart disease in adults.
For many children, normalization of blood pressure before adulthood could mitigate or even reverse long-term risk,” researchers note—a critical window during which interventions can have lifelong benefits.
5. Routine Screening Is Becoming a Global Priority

Despite the rising prevalence of pediatric hypertension, systematic blood pressure screening is not yet routine in many countries. A recent call from UK pediatricians advocates integrating blood pressure checks into school health programs, aligned with growth and vaccination assessments.
Importance of Regular Blood Pressure Screening
- Early detection enables early action.
- Many children with elevated blood pressure have no obvious symptoms.
- Detecting hypertension helps identify other underlying conditions that might have gone unnoticed.
In contexts such as India’s Karnataka state, where more than 7 lakh children were diagnosed with hypertension during a targeted screening, public health leaders have urged broader community awareness and education efforts.
6. Parental Awareness and Perception Gaps Remain Wide
Thriving public health programs depend on informed parents and caregivers. However, research reveals that many parents do not believe children can develop hypertension, which undermines early detection and prevention efforts. In one survey, 83% of parents thought children do not develop high blood pressure.
This gap clearly highlights the need for comprehensive educational campaigns specifically targeted at caregivers, aimed at improving understanding of childhood hypertension and its risks. In addition, stronger community health outreach initiatives are required to raise awareness, promote early screening, and encourage preventive behaviors at the local level. Most importantly, families must be empowered with practical knowledge about lifestyle-related risk factors—such as diet, physical activity, and weight management—so that informed decisions can be made to support long-term cardiovascular health in children.
By increasing awareness, communities can better advocate for screen-and-intervention policies in schools and clinics.
7. Genetic and Medical Causes Still Play a Critical Role
While lifestyle factors account for a large proportion of rising pediatric hypertension, secondary causes remain important, especially in younger children.
Secondary hypertension in children can result from a range of underlying medical conditions that directly affect blood pressure regulation. Common medical etiologies include kidney or renovascular diseases, which interfere with normal fluid and electrolyte balance, as well as endocrine disorders such as hormonal imbalances that disrupt cardiovascular control mechanisms. In addition, congenital heart defects may alter normal blood flow and pressure dynamics, while certain genetic syndromes are known to predispose children to persistently elevated blood pressure. Identifying these causes is essential, as secondary hypertension often requires targeted medical evaluation and condition-specific treatment rather than lifestyle modification alone.
Although rarer than lifestyle-associated primary hypertension, these conditions underscore the importance of medical evaluation in children with persistently elevated blood pressure.
8. Treatment Approaches Span Lifestyle and Medical Therapy
Just as the risk factors for childhood hypertension vary, treatment strategies are also individualized, with lifestyle interventions serving as the first line of management for most children. Non-pharmacologic measures are typically prioritized and include adopting healthier dietary habits, such as reducing sodium intake and ensuring balanced nutrition, alongside increasing regular physical activity. In addition, reducing excessive screen time is encouraged to support more active daily routines, while structured weight management programs may be implemented for children who are overweight or obese. Collectively, these interventions aim to normalize blood pressure levels while promoting long-term cardiovascular health.
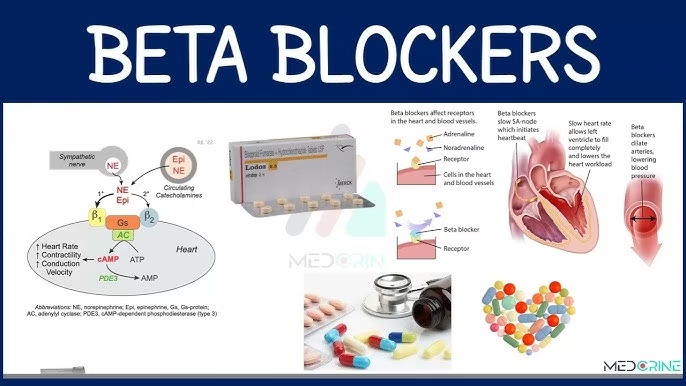
Medical management becomes necessary in cases of stage 2 hypertension or when elevated blood pressure persists despite consistent lifestyle modifications. Under professional medical guidance, pharmacologic therapy may be introduced to achieve adequate blood pressure control and reduce the risk of complications. Physicians commonly prescribe medications such as ACE inhibitors, beta-blockers, or calcium channel blockers, with the specific choice determined by individual factors including the child’s age, underlying conditions, severity of hypertension, and overall clinical profile.
Given the complexity and evolving guidelines, treatment should be tailored by pediatric specialists experienced in blood pressure management.
9. Social and Environmental Contexts Shape Risk
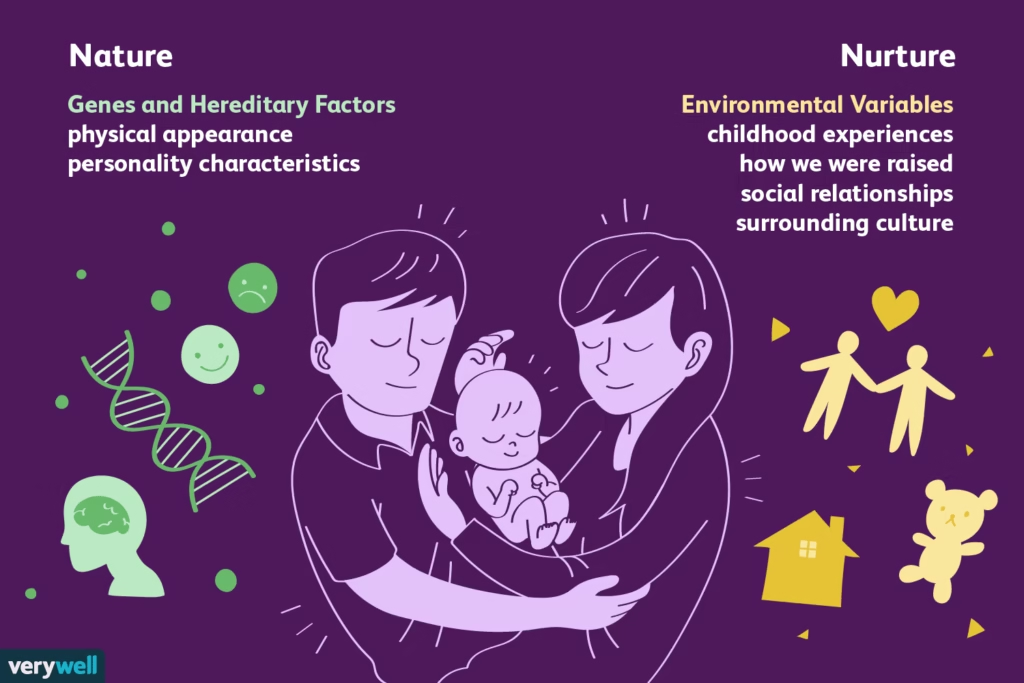
Beyond individual behaviors, broader societal and environmental factors play a significant role in the development of childhood hypertension. Exposure to urban pollution and various environmental stressors can directly and indirectly affect cardiovascular health, while limited access to nutritious foods in food deserts and socioeconomic disparities can exacerbate poor dietary habits. Additionally, adverse childhood experiences (ACEs), including household instability, trauma, and chronic stress, have been linked to elevated blood pressure and long-term cardiovascular risk. These factors highlight that childhood hypertension is not solely a result of personal choices but is also shaped by the broader social and environmental context in which a child grows up.
Indeed, research links cumulative ACEs with higher adult blood pressure, suggesting that childhood experiences can shape cardiovascular health trajectories over a lifetime.
These findings call for integrated approaches that combine medical care with social support and healthy environments.
10. Technological and Policy Innovations Offer Hope

Finally, innovations in health technology and policy are beginning to create new opportunities:
Digital health tools are increasingly being explored as a means to enhance the monitoring and management of childhood hypertension. Wearable devices and app-based blood pressure monitors, once validated for pediatric use, have the potential to track blood pressure trends continuously and provide real-time data outside of traditional clinical settings. By enabling more frequent and convenient monitoring, these tools can support early detection, improve adherence to treatment plans, and facilitate timely intervention, ultimately contributing to better long-term cardiovascular outcomes for children.
School and community policies play a crucial role in preventing and managing childhood hypertension. Increasing evidence supports initiatives such as reducing salt content in school meals, which can help lower dietary sodium intake and support healthy blood pressure levels. Additionally, implementing mandatory physical education programs ensures that children engage in regular physical activity, promoting cardiovascular fitness and overall health. Community-based programs that encourage active lifestyles further reinforce these efforts by providing accessible opportunities for exercise and healthy habits outside of school, creating an environment that supports long-term blood pressure management and wellness.
These strategies align with global efforts to curb rising lifestyle-related diseases in younger populations.
Conclusion
Childhood hypertension represents a pressing and increasingly prevalent public health challenge with implications that extend well into adulthood. The rising rates of elevated blood pressure among children, fueled by lifestyle factors, environmental influences, and underlying medical conditions, underscore the urgent need for early detection, preventive interventions, and comprehensive management strategies. Fortunately, evidence shows that proactive measures—including routine screening, family education, lifestyle modifications, medical treatment when necessary, and supportive school and community policies—can significantly reduce long-term cardiovascular risks. By addressing both individual behaviors and broader societal determinants, healthcare providers, parents, and policymakers have a critical opportunity to safeguard children’s heart health today and promote healthier adult populations in the future.
Read the latest trending HEALTH news here.
![]()



