Introduction
Gestational diabetes mellitus (GDM) has emerged as one of the most closely studied pregnancy-related conditions in modern maternal healthcare. As global rates of obesity, delayed pregnancies, and metabolic disorders continue to rise, the prevalence of GDM has increased steadily, placing both mothers and infants at heightened risk for short- and long-term complications. Traditionally, diagnosis and management have relied on standardized glucose testing and lifestyle interventions; however, these approaches have often fallen short in addressing individual risk profiles and early disease development.
In recent years, significant advances in medical research, digital health, and data science have reshaped how gestational diabetes is understood, detected, and managed. From continuous glucose monitoring and artificial intelligence-driven prediction models to novel biomarkers and precision medicine strategies, innovative solutions are being developed to support earlier diagnosis, personalized care, and improved pregnancy outcomes. This article explores the top 10 innovations in gestational diabetes research, highlighting how current scientific breakthroughs are transforming clinical practice and setting new standards for maternal and fetal health in 2026 and beyond.
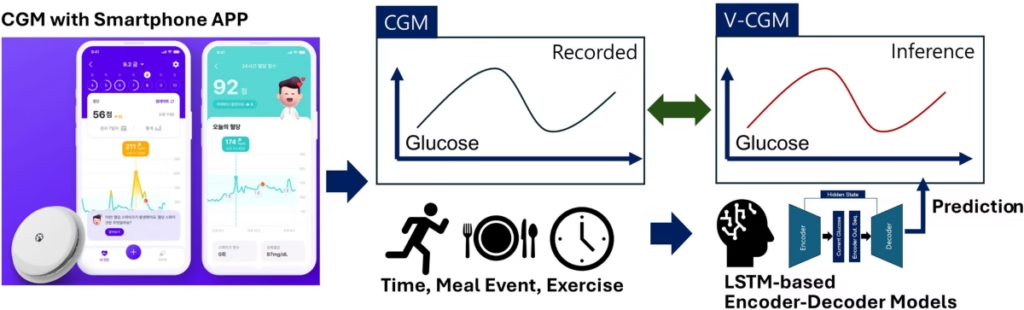
1. Continuous Glucose Monitoring (CGM): Redefining Glucose Control in Pregnancy

Continuous glucose monitoring (CGM) devices have rapidly moved from an emerging technology to one of the most widely validated tools in GDM care. Unlike traditional finger-stick measurements, CGMs provide real-time glucose data throughout the day — including overnight and post-meal trends that were previously unmeasurable.
Continuous glucose monitoring (CGM) plays a critical role in gestational diabetes management because it delivers measurable improvements in both glycemic control and pregnancy outcomes. A 2025 randomized controlled trial demonstrated that pregnant individuals with GDM achieved a significantly higher percentage of time in the target glucose range when real-time CGM was used instead of conventional capillary blood glucose monitoring alone. In addition, multiple clinical trials have shown that early CGM use is associated with lower rates of large-for-gestational-age infants, reduced preterm births, and fewer neonatal intensive care unit admissions. Beyond management benefits, advanced CGM-derived metrics have also been shown to outperform traditional risk models in predicting gestational diabetes at earlier stages, particularly among high-risk populations, supporting its growing role in both prevention and personalized care.
However, while CGM technologies are valuable, research continues to refine their optimal use and validate specific pregnancy-targeted metrics before universal adoption in all GDM cases.
2. Novel Biomarkers for Early Detection and Risk Stratification
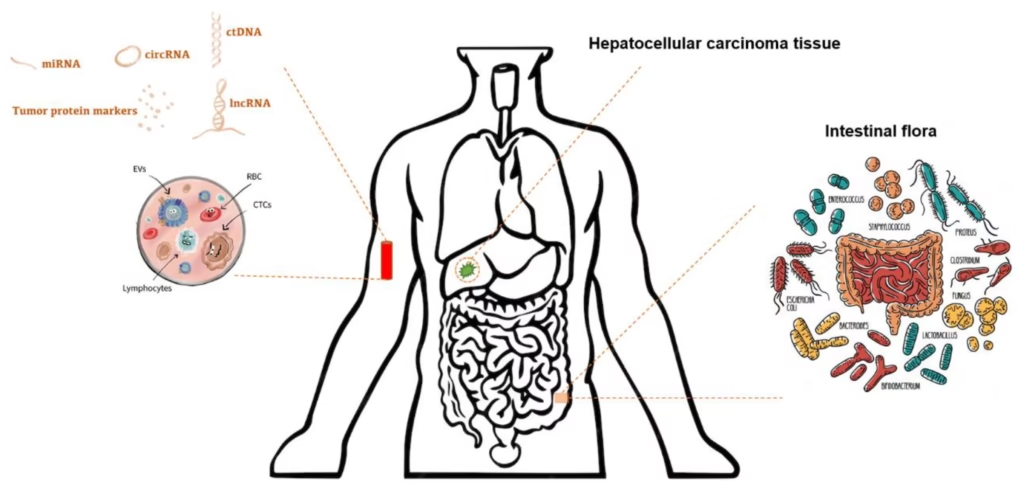
Research into biological markers (biomarkers) that signal the risk of GDM before clinical diagnosis is gaining traction, with potential to reshape screening guidelines.
Recent breakthroughs in biomarker science have significantly advanced the early detection and risk stratification of gestational diabetes mellitus. Early 2026 studies have identified specific circulating microRNAs, particularly miR-326 and miR-532-3p, as highly promising biomarkers due to their strong diagnostic accuracy in detecting GDM at earlier stages of pregnancy. In parallel, metabolic and inflammatory markers have gained attention, with elevated levels of branched-chain amino acids (BCAAs) and pro-inflammatory cytokines such as TNF-α and IL-6 demonstrating predictive value for the later development of GDM, often revealing underlying metabolic dysfunction well before clinical symptoms emerge. Additionally, adipokines and cytokines—including chemerin, resistin, and omentin-1—are being actively studied for their roles in glucose metabolism and insulin sensitivity, further strengthening their potential use in early screening and personalized risk assessment.
Development and validation of a panel of early-stage biomarkers could enable predictive rather than reactive care — identifying women at high risk before glucose intolerance becomes clinically measurable.
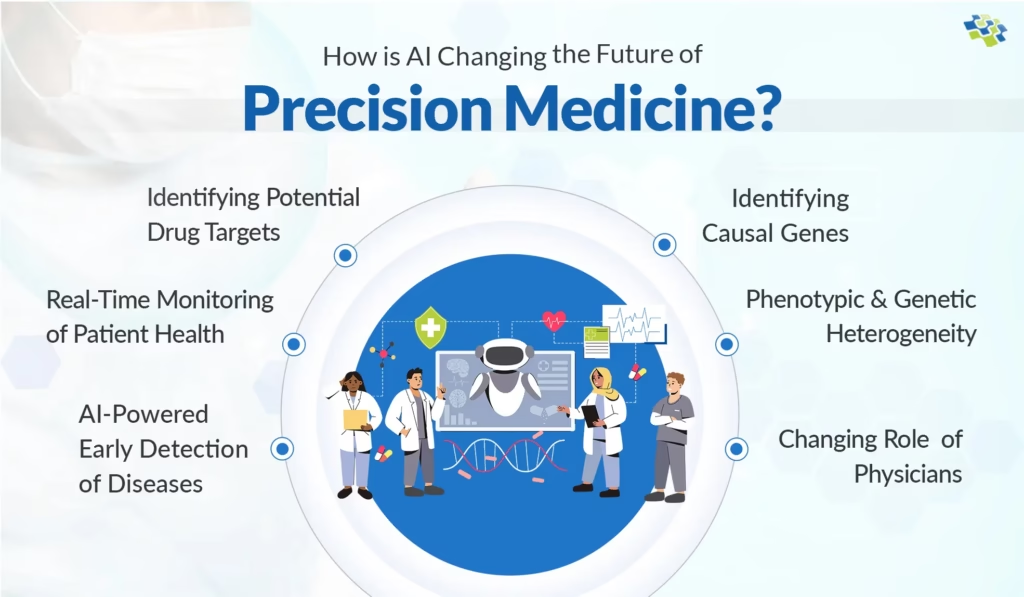
3. Artificial Intelligence and Machine Learning in GDM Prediction

AI and machine learning (ML) are transforming how researchers interpret complex data and foresee gestational metabolic changes.
Smart analytics are increasingly fueling precision care in gestational diabetes research, driven by extensive evaluations of artificial intelligence–based prediction models. Researchers have reviewed more than 70 studies examining AI systems that assess GDM risk using a wide range of variables, including maternal demographics, clinical history, biochemical markers, and wearable sensor data. Findings consistently show that advanced neural networks and tree-based machine learning models outperform traditional prediction algorithms in identifying high-risk pregnancies. However, despite their strong predictive performance, challenges related to reproducibility, data standardization, and clinical readiness remain, highlighting the need for further validation before widespread implementation in routine prenatal care.
These tools are designed to enhance gestational diabetes care by delivering personalized risk scores derived from multi-dimensional data, including clinical history, metabolic markers, and digital health inputs. By integrating early pregnancy indicators, they enable preemptive diagnosis and risk identification well before traditional screening windows. In addition, automated alerts can be generated within electronic health record (EHR) systems, allowing clinicians to receive timely notifications, intervene earlier, and make data-driven decisions that improve monitoring efficiency and patient outcomes.
Machine learning systems also enhance CGM usage by identifying metabolic subphenotypes that tailor dietary, lifestyle, and pharmacologic interventions.
4. Precision Medicine – Tailored Treatments and Subphenotype Identification
Precision medicine is moving beyond one-size-fits-all approaches by defining distinct GDM subtypes, each with specific metabolic drivers and tailored care pathways.
Glycemic and metabolic profiling is playing a key role in advancing precision medicine for gestational diabetes, as research initiatives such as the GDM-CARE project investigate the integration of detailed glycemic patterns with metabolic biomarker data. By analyzing these combined profiles, researchers are able to identify the heterogeneity within GDM, recognizing that the condition does not present uniformly across all patients. This approach allows for the differentiation of distinct subtypes, such as insulin resistance–dominant profiles versus those driven primarily by β-cell dysfunction, enabling treatments to be more accurately matched to individual metabolic needs and improving the effectiveness of clinical interventions.
This direction promises better outcomes by aligning care strategies (diet, medication, monitoring) with personalized risk profiles rather than relying solely on generic glucose thresholds.
5. Telemedicine and Connected Digital Health Platforms

Digital health innovations are reshaping how GDM is monitored and managed — particularly through remote patient engagement.
Key advancements in digital health for gestational diabetes management include the expansion of telemedicine platforms that allow physicians to review glucose data in real time, improving responsiveness and continuity of care. In parallel, smartphone applications have been developed to support daily diet logging, physical activity monitoring, and glucose tracking, making self-management more accessible and structured for pregnant individuals. These tools are increasingly being integrated with clinical decision support systems (CDSS) that leverage sensor data and artificial intelligence insights to recommend insulin dose adjustments or dietary modifications, delivering real-time feedback that supports timely, data-driven clinical decisions.
These tools help reduce clinic visits, enhance patient engagement, and support dynamic management plans evolving with pregnancy physiology.
6. Metabolomics and Multi-Omics for Deeper Biological Insights
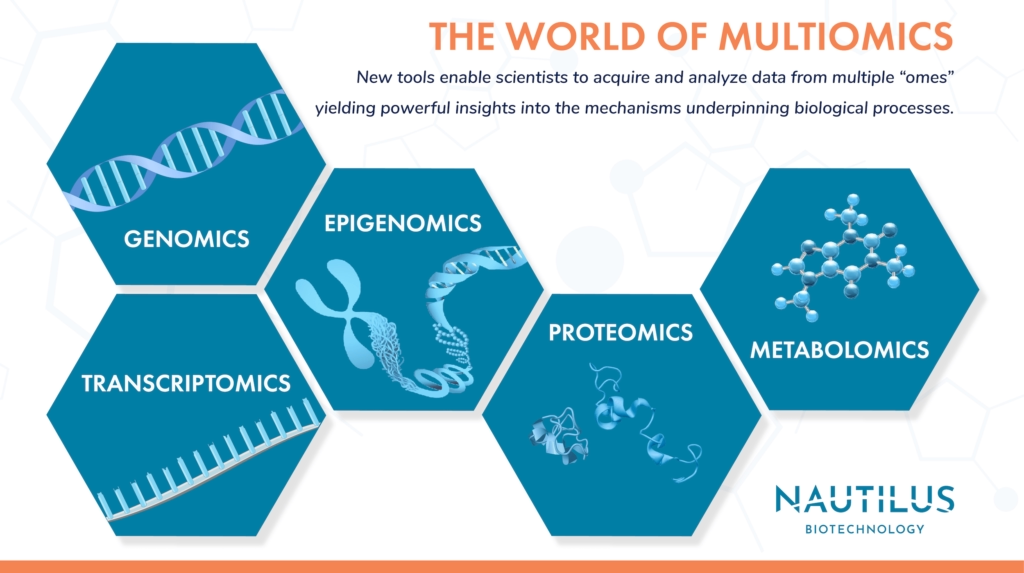
Multi-omics technologies — including metabolomics, genomics, and proteomics — are enabling researchers to understand the biological foundations of GDM at unprecedented depth.
These advances have important implications for gestational diabetes research and care, as they enable a deeper understanding of the biological mechanisms underlying the condition. The identification of specific metabolic signatures associated with insulin resistance allows for earlier recognition of at-risk pregnancies and more targeted interventions. At the same time, improved insight into genetic contributors to maternal glucose regulation is helping explain individual susceptibility to GDM. In addition, mapping the hormonal and inflammatory pathways that drive GDM pathophysiology is clarifying how metabolic, immune, and endocrine factors interact during pregnancy, supporting the development of more precise diagnostic tools and personalized treatment strategies.
By elucidating molecular mechanisms, this research paves the way for targeted preventive strategies and molecular subtyping of GDM.
7. Education and Behavioral Tools Based on Real-World CGM Use

While remote monitoring is a key innovation, CGM devices also function as educational tools for pregnant patients, helping them understand how behaviors influence glucose patterns.
Earlier research has shown that continuous glucose monitoring (CGM) assistance can significantly enhance patient engagement and self-management in gestational diabetes care. By providing continuous, real-time glucose data, CGM improves awareness of glycemic variability and helps individuals better understand how meals, physical activity, and daily routines affect blood sugar levels. This immediate feedback has been shown to motivate meaningful dietary and lifestyle adjustments, while also encouraging the development of healthier self-management habits through clear, tangible insights that reinforce positive behavioral changes throughout pregnancy.
This behavioral aspect—often overlooked—plays a central role in sustained glucose control throughout pregnancy.
8. New Diagnostic Algorithms and Risk Scores
Traditional gestational diabetes screening (e.g., oral glucose tolerance testing) has limitations in sensitivity, timing, and convenience.
Emerging research in gestational diabetes is increasingly focused on integrating multiple data sources to improve early detection and personalized care. Continuous glucose monitoring (CGM)-derived metrics provide detailed insights into daily and postprandial glucose patterns, while biomarker signatures offer information about underlying metabolic and inflammatory processes. When combined with machine learning–based risk scores, these approaches enable more accurate prediction of GDM development, allowing clinicians to identify high-risk pregnancies earlier and tailor interventions to individual patient profiles.
These combined strategies can improve early diagnosis and predict failure of standard screening techniques, particularly in diverse populations with varying ethnic, metabolic, and lifestyle profiles.
9. Understanding Long-Term Progression to Type 2 Diabetes
Gestational diabetes significantly raises the risk of T2DM post-pregnancy. Recent research has identified distinct molecular drivers underlying progression from GDM to T2DM — offering new targets for prevention after delivery.
An improved understanding of metabolic trajectories and molecular phenotypes could lead to earlier intervention strategies for women after childbirth — slowing or preventing the emergence of chronic diabetes later in life.
10. Emerging Therapeutics and Glucose-Responsive Treatments
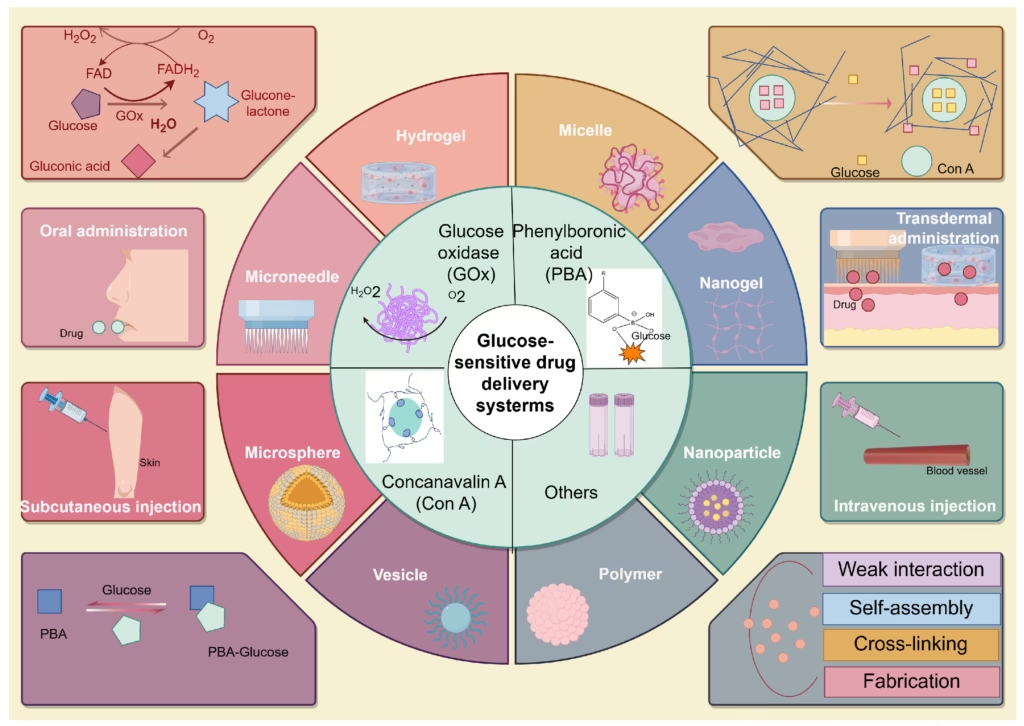
Although lifestyle management remains the first-line therapy, research into novel pharmacologic solutions continues.
Key developments in general diabetes research that hold potential relevance for gestational diabetes include the creation of glucose-sensitive insulin analogues, which can dynamically adjust their activity in response to blood sugar levels, offering more precise and responsive glucose control. In addition, oral insulin formulations are being developed to improve ease of administration and enhance patient adherence, while simultaneously reducing the risk of hypoglycemia. These innovations represent promising avenues for future GDM therapies, with the potential to provide safer, more convenient, and more effective management options for pregnant individuals.
While most of these remain in broader diabetes research pipelines rather than GDM-specific approvals, they represent promising future additions to the gestational diabetes therapeutic landscape.
Final Thoughts
Gestational diabetes research is undergoing a transformative period, driven by technological innovation, molecular discoveries, and precision medicine approaches. From continuous glucose monitoring and AI-driven predictive models to novel biomarkers, metabolomic profiling, and digital health platforms, these advancements are reshaping how GDM is detected, monitored, and managed. Personalized strategies—tailored to individual metabolic profiles and supported by real-time data—are improving both maternal and neonatal outcomes, while early detection tools and risk stratification methods offer the potential to prevent complications before they arise. Emerging therapeutics, including glucose-sensitive insulin analogues and oral insulin formulations, further expand the future possibilities for safer and more effective treatment. Collectively, these innovations underscore a shift toward proactive, data-driven, and individualized care in gestational diabetes, offering hope for healthier pregnancies and long-term metabolic health for both mothers and their children.
Explore the latest trending HEALTH news here.
![]()