Introduction
Influenza has long been regarded as a familiar seasonal illness; however, recent global developments suggest that the nature of the flu is changing. In the past few years, emerging influenza strains have been identified across multiple regions, raising renewed concern among scientists, healthcare professionals, and public health authorities. These new strains are not only evolving more rapidly but are also demonstrating unusual patterns of transmission, severity, and resistance, making them significantly more complex than traditional seasonal flu viruses.
As global travel resumes at full scale, animal-to-human interactions increase, and viral mutations continue to accelerate, the risk posed by emerging flu strains has intensified. Reports from international health organizations indicate rising flu activity driven by newly identified variants, alongside sporadic human infections linked to avian influenza viruses. Although widespread human-to-human transmission has not yet been confirmed for many of these strains, the growing frequency of detections has highlighted vulnerabilities in global preparedness systems.
This article explores the top 10 risks of the emerging flu strain, offering a comprehensive, evidence-based analysis grounded in current events and verified public health data. By examining these risks in detail, readers will gain a clearer understanding of why emerging influenza strains represent a serious public health concern and why proactive awareness, surveillance, and prevention remain essential in today’s interconnected world.
Risk #1 — Viral Mutation and Genetic Shift
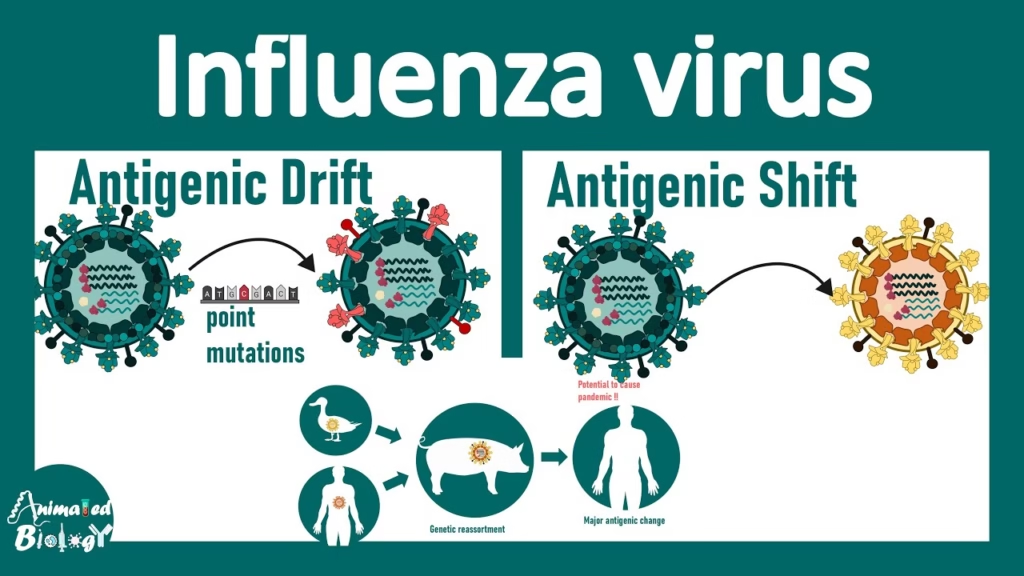
One of the most significant risks of emerging flu strains is the ability of influenza viruses to mutate rapidly. These mutations can occur at the genetic level in two main ways:
1. Antigenic Drift — Small genetic changes over time.
2. Antigenic Shift — Major genetic reassortment leading to new viral types.
Both processes can produce influenza viruses that evade immune protection from prior infection or vaccination.
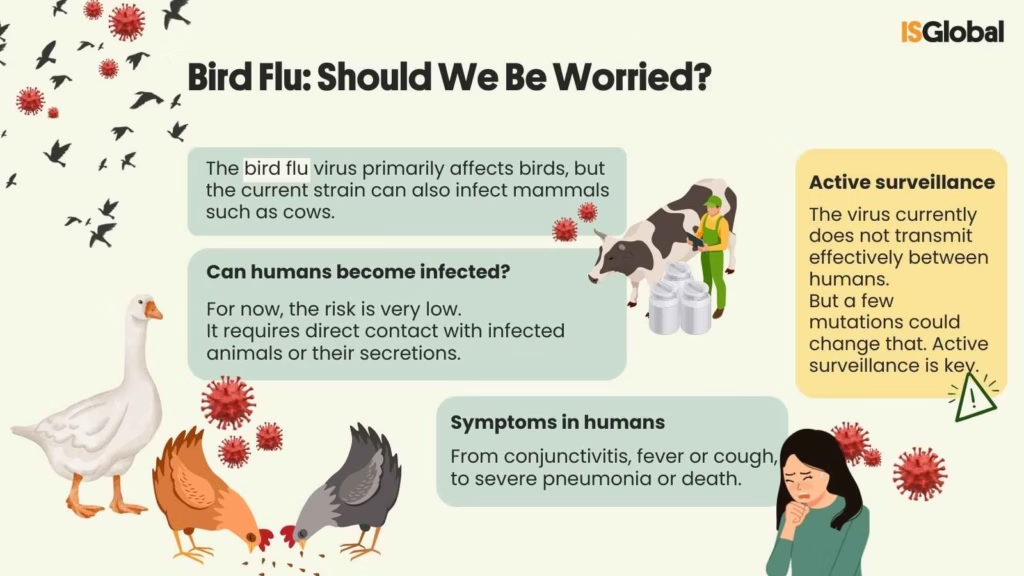
A recent study has highlighted a critical concern regarding the H5N1 “bird flu” virus, indicating that even a single genetic mutation may significantly enhance its ability to bind to human cellular receptors, a key biological step toward potential human-to-human transmission. As a result, this mutation-driven risk carries two major consequences: first, increased infectivity, as emergent strains may gain the capacity to infect a broader range of hosts, including humans; and second, immune escape, whereby new variants may diminish the effectiveness of pre-existing immunity and seasonal vaccines. Taken together, this ongoing genetic evolution has the potential to transform relatively contained outbreaks into more widespread and consequential public health threats.
Risk #2 — Zoonotic Spillover from Animals to Humans
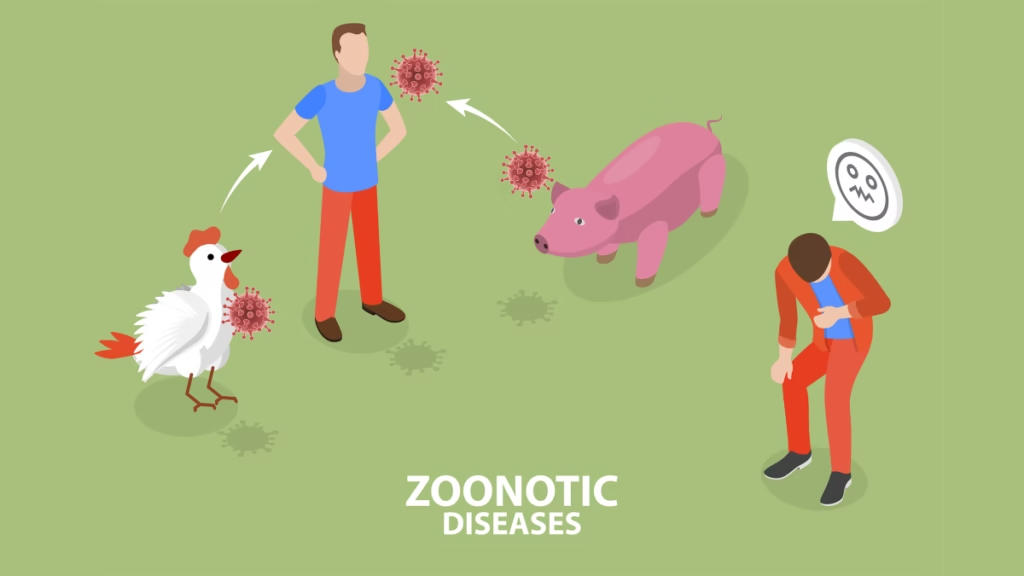
The second major risk with emerging flu strains involves zoonotic transmission — where viruses move from animals to humans. Influenza viruses circulate widely in wild birds, poultry, and increasingly, other mammals.
In the Americas and beyond, avian influenza A(H5N1) viruses continue to circulate in wild birds and domestic animals, including dairy cattle.
This development matters because wild birds, particularly waterfowl, serve as natural reservoirs for influenza A viruses, allowing these pathogens to persist and evolve in the environment. At the same time, agricultural exposure places poultry and livestock workers at heightened risk due to frequent and direct contact with infected animals. Moreover, documented cases of cross-species transmission are increasing, with humans becoming infected through close interaction with affected animals, underscoring the growing public health implications of zoonotic spillover events.
Notably, WHO reported a human infection with H5N5 in late 2025 — the first globally confirmed case from this subtype. Although human-to-human transmission has not been observed in this case, it emphasizes the continued risk of animal viruses crossing the species barrier.
Occupational exposure — to poultry, dairy cattle, or wild animals — remains a leading cause of zoonotic infection. Strengthening surveillance at this human-animal interface is essential to detect early changes.
Risk #3 — Co-Circulation with Seasonal Flu Variants
In addition to emerging strains like avian influenza subtypes, typical seasonal influenza viruses are actively circulating. This dual circulation multiplies risk because co-infection can lead to viral reassortment, where two different influenza viruses exchange genetic material.
In the 2025–2026 season, public health monitoring has indicated:
- A significant rise in influenza illness driven by H3N2 subclade K viruses, which appeared after vaccine formulation decisions were finalized.
- Reports of flu activity climbing to high levels in regions like the United States, especially when combined with other respiratory viruses.
When two or more distinct influenza viruses circulate simultaneously within a population, the likelihood of genetic reassortment increases, creating conditions under which novel influenza strains may emerge. Historically, reassortment has been a recognized pathway for the development of pandemic influenza viruses, as genetic material is exchanged between different viral strains. Consequently, this ongoing dual circulation presents layered risks, including the potential emergence of recombinant influenza variants with unknown transmissibility, severity, or immune response profiles, as well as increased pressure on public health surveillance systems that must accurately detect, monitor, and differentiate among multiple co-circulating viruses.
Risk #4 — Increased Human Cases of Avian Flu Subtypes
While human infection with avian influenza viruses remains rare, the number of cases documented globally has risen, particularly in countries with ongoing bird outbreaks. For example:
- Between 2024 and 2025, WHO reported dozens of human cases of H5N1 infection in multiple countries, including Cambodia, China, and the United States.
- Some regions have documented human infections with other avian subtypes, such as H9N2 and H10N3, indicating diverse influenza reservoirs.
Importantly, although sustained person-to-person transmission has not yet been documented, each new human case represents an opportunity for further adaptation.
Key implications include a significant case fatality risk, as certain avian influenza strains, such as H5N1, have demonstrated high mortality rates in humans, according to the World Health Organization. In addition, the public health response is inherently complex, as effective detection, isolation, and contact tracing of human cases require strong clinical capacity and advanced laboratory infrastructure. Furthermore, although the absence of sustained person-to-person transmission has kept most outbreaks sporadic, the risk of viral mutation during human infection persists, maintaining the potential for more efficient transmission in the future.
Thus, human cases of avian influenza are significant events that merit heightened attention, even if they are currently uncommon.
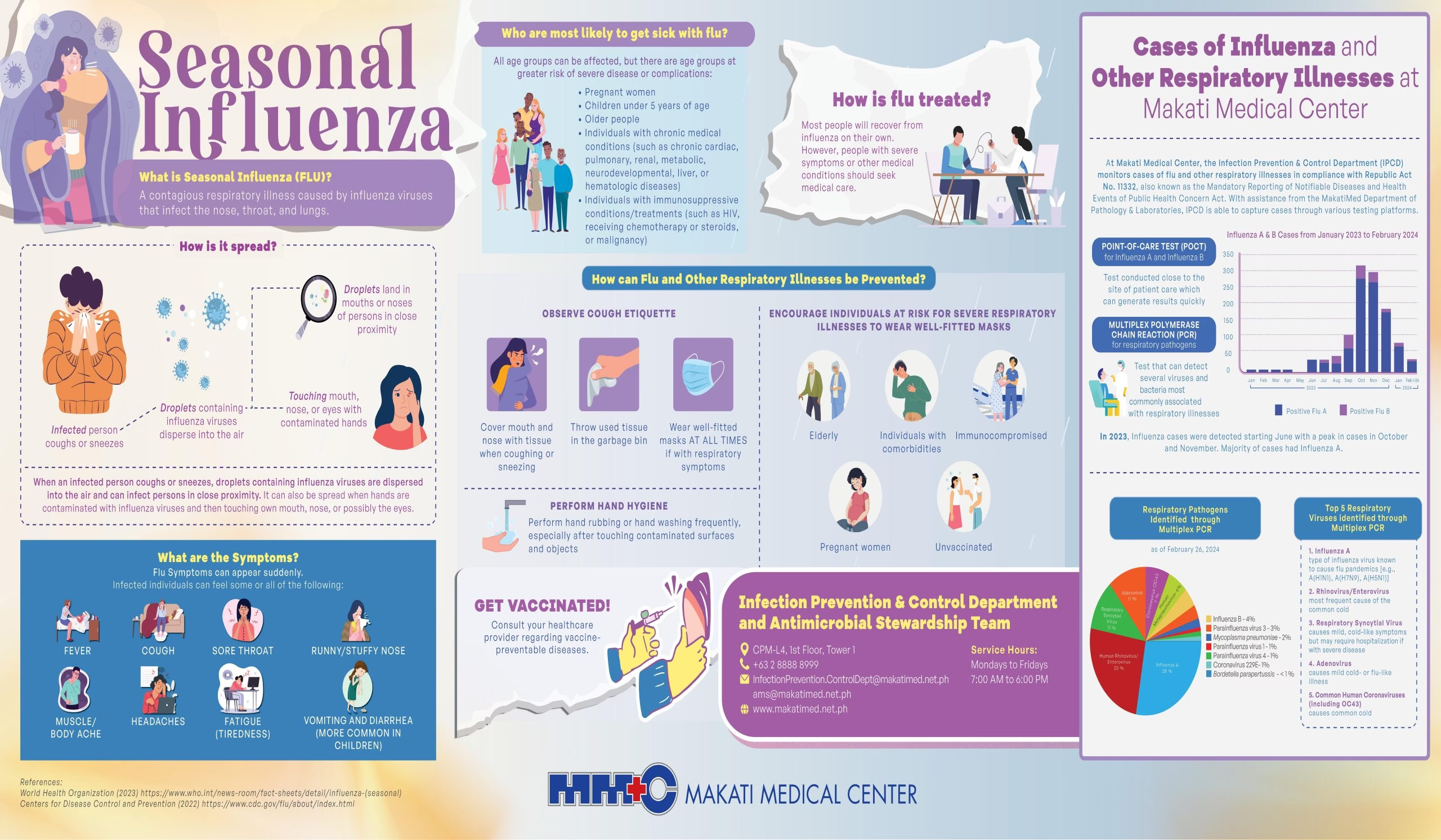
Risk #5 — Resistance to Existing Vaccines

Seasonal flu vaccines are reformulated annually based on predictions about circulating strains. However, timing matters. The emergence of novel variants after vaccine strain selection can result in a mismatch, reducing vaccine effectiveness.
In the 2025–2026 flu season:
- The H3N2 subclade K strain emerged after the vaccine formula was already finalized.
- This timing raised concern among epidemiologists because the circulating strain differed substantially from the predicted one used to manufacture vaccines.
Vaccine mismatch can result in lower levels of protection against infection, increased rates of severe illness and hospitalization, and greater viral spread within communities. Although seasonal influenza vaccines generally continue to provide partial protection against severe disease, this growing mismatch trend underscores the importance of adaptive vaccine technologies and accelerated manufacturing methods that are capable of responding rapidly to the ongoing evolution of influenza strains.
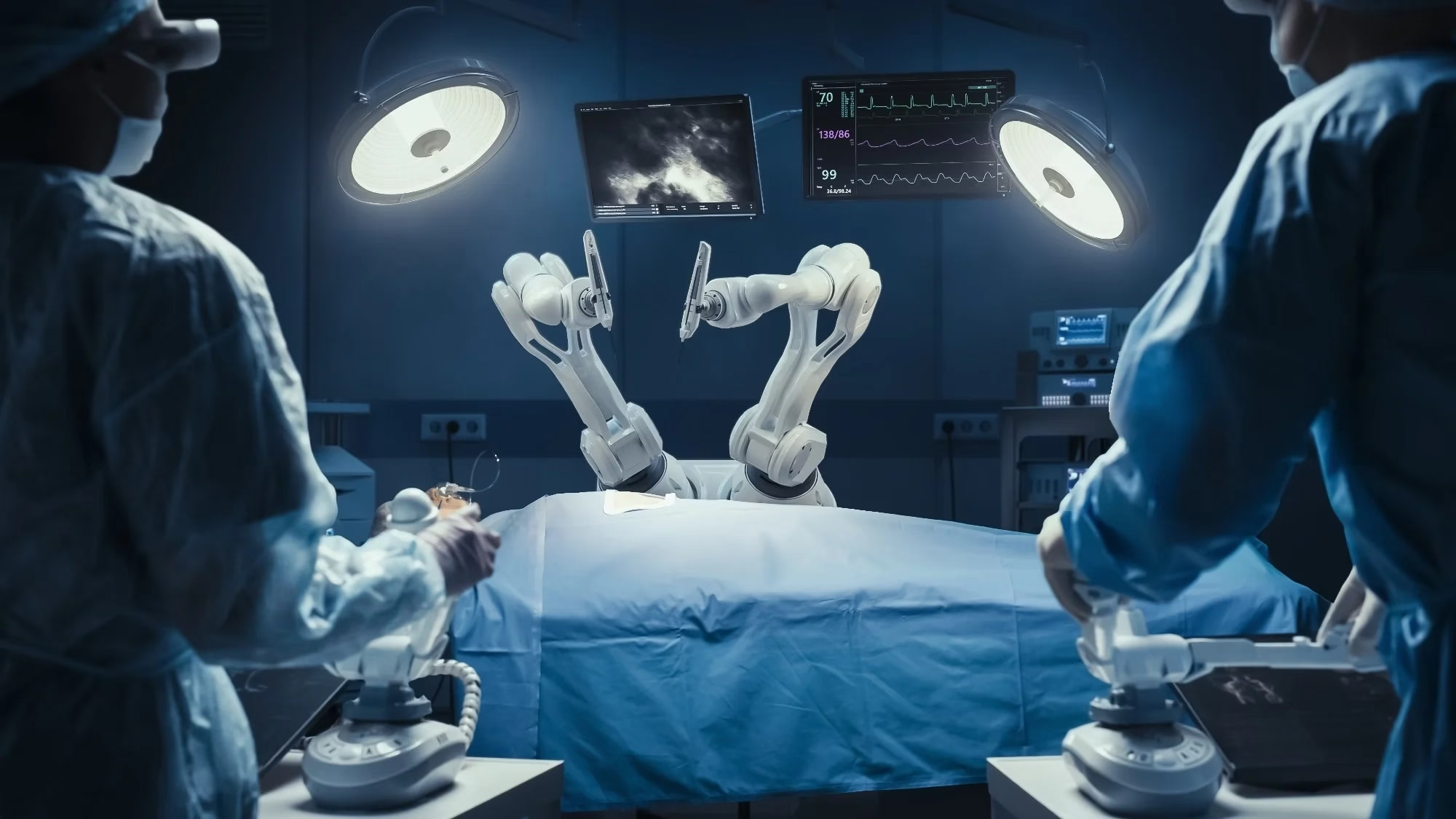
Risk #6 — Healthcare System Strain

The arrival of an aggressive influenza wave, particularly one involving emergent strains, can place substantial strain on healthcare systems, a risk that is further amplified when seasonal influenza activity coincides with other circulating respiratory infections such as respiratory syncytial virus (RSV) and SARS-CoV-2. In the United States and other high-income countries, elevated levels of respiratory virus activity have been reported, largely driven by influenza and RSV, while influenza-related hospitalizations have increased markedly, compounding pressure on hospitals, workforce capacity, and critical clinical resources.
Healthcare systems face an increased burden as a result of hospital and intensive care unit bed shortages, staffing constraints driven by illness and workforce burnout, and ongoing supply challenges affecting the availability of antiviral medications and critical diagnostic reagents.
The combination of complex surveillance requirements and patient care demand underscores why emergent flu strains represent not just a biological risk, but a systemic health system risk.
Risk #7 — Diagnostic and Surveillance Challenges
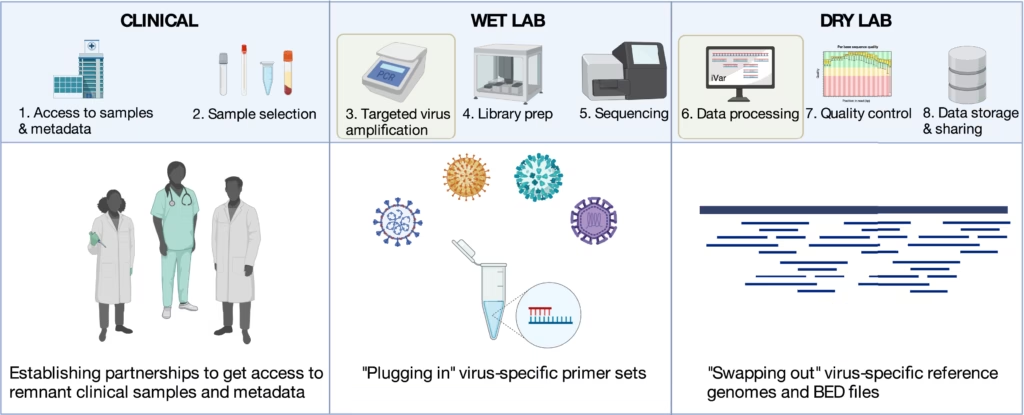
The detection and tracking of influenza strains depend upon laboratory capacity, genomic sequencing, and coordinated reporting.
For emerging strains, major diagnostic challenges include:
- Differentiation among flu subtypes, including novel avian strains.
- Genomic surveillance capacity, which varies by country.
- Timeliness of data sharing, which affects global response efforts.
Global surveillance networks have identified new subtypes like H5N5, but ongoing monitoring is essential to detect changes in transmission or virulence.
Furthermore, differing surveillance capabilities between high-income and low-income countries can result in data gaps, obscuring real global risk levels.
Strengthening surveillance infrastructure, expanding genomic sequencing, and harmonizing reporting systems remain critical priorities to reduce this risk.
Risk #8 — Public Misinformation and Risk Perception
Public understanding of influenza and emerging variants is shaped by media coverage, social media discourse, and official health messaging. One challenge in 2026 has been how nuanced risk assessments (e.g., “low risk to general public”) are perceived by the broader population.
Misinformation can have serious consequences by fueling unnecessary panic or, conversely, complacency among the public, encouraging resistance to vaccination campaigns, and leading to the misinterpretation of critical public health guidance, all of which can undermine efforts to control the spread of infectious diseases.
Accurate, transparent communication from health authorities is essential to ensure that individuals take appropriate protective measures without undue fear.
Risk #9 — Economic and Food Security Impacts

Influenza outbreaks among domestic animals — particularly poultry and dairy cattle — carry economic and food security implications.
Large-scale outbreaks can lead to:
- Culling of livestock or poultry herds.
- Disruption of supply chains for meat and dairy products.
- Trade restrictions and export bans.
For farmers and rural communities relying on livestock, these impacts can be profound.
Emerging strains that continue to circulate widely in animals, as documented across the Americas, highlight the intersection of agricultural health and public health.
Risk #10 — Pandemic Potential and Long-Term Outcomes
Finally, the most significant overarching risk posed by an emerging influenza strain is its pandemic potential—that is, the possibility that a virus could acquire sustained human-to-human transmission and spread globally. Although this scenario has not yet occurred with avian influenza strains or reservoir strains such as the H3N2 subclade K, the possibility remains, underscoring the need for ongoing vigilance and preparedness.
Several factors contribute to pandemic risk:
- Genetic reassortment between avian and human strains.
- High global travel and interconnected populations.
- Inadequate vaccine match and surveillance gaps.
Pandemics can cause long-term societal disruption, extensive morbidity and mortality, and economic instability. Preparedness planning, investment in vaccine platforms, and robust global cooperation are essential measures to mitigate this ultimate risk.
Conclusion: Navigating Uncertainty with Preparedness
Influenza will always be a challenge because of its ability to evolve, cross species, and adapt to new environments. Yet the emerging strains of 2025–2026 have underscored the urgency of comprehensive pandemic preparedness.
The risks outlined in this article — from viral mutation to healthcare strain and pandemic potential — are real, documented, and grounded in current surveillance data. While public health systems globally continue to monitor and respond, individual actions remain vital: vaccination, staying informed through reliable sources, and maintaining general respiratory health practices.
By understanding the top risks of emerging influenza strains, societies can better equip themselves for both the present flu season and the unpredictable future that lies beyond.
Click here to read more trending HEALTH news.
![]()